55year old male with c/o SOB (grade 4), decreased urine output and pedal edema
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
Patient came to the casualty with c/o SHORTNESS OF BREATH (grade 4) since 1day
Decreased urine output since 3days
Pedal edema since 3days
HOPI:-
Patient was apparently asymptomatic 10years back then he developed oedema in both legs which was relieved on medication.
6years back patient has a h/o fall which led to the fracture of right leg which was treated conservatively. Since then patient walks with STICK support
5years back patient came with Similar complaints which was intermittent episodes of pedal edema which was pitting type and patient has been diagnosed as RENAL FAILURE and has been treated conservatively.
2years back patient has a h/o fall which led to the fracture of left leg which was treated conservatively. Since then patient walks with 2STICKS
Similar complaints happened on 15/7/23 and was treated conservatively
3days back pt had decreased urine output,pedal edema which was pitting type extending upto knee. Pt has SOB GRADE 4 since 1dat which is insidious in onset, gradually progressive and also abdominal distension which is non-tender.
3DAYS back pt has developed itching on the right hand which lead to ulceration and has been treated conservatively.
PAST HISTORY:-
K/C/O CKD
K/C/O SPONDYLOARTHROPATHY
Not a K/C/O DM,HTN,TB,ASTHMA
PERSONAL HISTORY -
mixed diet
Normal appetite
Regular Bowel and Bladder movements
Sleep -adequate
No allergies
addictions- ALCOHOL CONSUMER ONCE A WEEK (180ML)
FAMILY HISTORY:- NOT SIGNIFICANT
GENERAL EXAMINATION
Patient is conscious coherent and cooperative
No signs of pallor, icterus, cyanosis, clubbing ,lymphadenopathy
Vitals-
Temp- Afebrile
BP-122/60 mm of Hg
PR-122bpm
RR-27cpm
Spo2 -83% on room air
97%ON 3LITS OF O2
GRBS-93mg/dl
SYSTEMIC EXAMINATION
CVS-s1,s2 heard,no murmurs
Rs-BAE +,NVBS
P/A-
SOFT,
Non tender
ABDOMINAL GRITH-78 cm
CNS- NAD
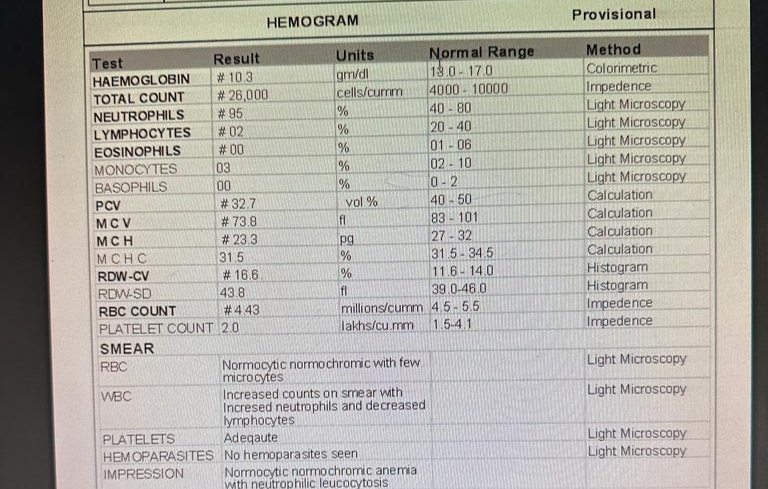
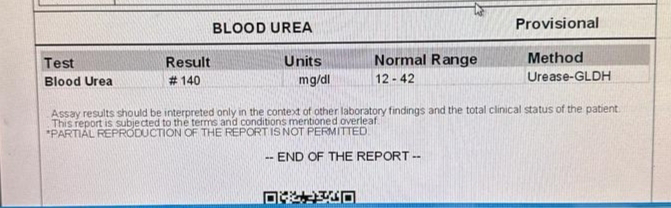
INVESTIGATIONS
PROVISIONAL DIAGNOSIS
SEPTIC SHOCJ WITH MODS
RT UPPER LIMB CELLULITIS
RIGHT HEART FAILURE
AKI ON CKD
HAEMODIALYSIS (1ST SESSION DONE IN 31/7/23)
TREATMENT
1) INJ. MEROPENEM 1GM IV/BD
2) INJ. CLINDAMYCIN 600MG IV/TID
3) INJ. PAN 40MG IV/OD
4) INJ. NORAD 23ml/HR (46ML NS+4ML NORAD) INCREASE OR DECREASE ACCORDING TO MAP
5) INJ. VASOPRESSIN 3.2ML/HR INCREASE OR DECREASE ACCORDING TO MAP
6) INJ. DOBUTAMINE 2ML/HR INCREASE OR DECREASE ACCORDING TO MAP
7) INJ. 25D IV/STAT IF GRBS <70MG/DL
8) INJ. LASIX 40MG IV/BD IF SBP >110MMHG
9) TAB NODOSIS 500 PO/BD
10) INJ. EPO 4000 IU sc WEEKLY ONCE
11) TAB SHELCAL-CT PO/OD
12) TAB VIT C PO/OD
13) TAB CHYMOROL FORTE PO/TID
14) RT UL ELEVATION
15) BP PR SPO2 MONITORING HOURLY